From cure to care
Chronic conditions are now the leading cause of death and disability worldwide. Disease rates from these conditions are accelerating globally, and impacting all socioeconomic classes. This has shifted the focus for health services from ‘cure’ to health ‘care’.
12 chronic conditions pose a significant burden in terms of morbidity, mortality and health care costs in Australia, and importantly, are amenable to preventive measures:
- coronary heart disease
- stroke
- asthma
- lung and colorectal cancer
- depression
- type 2 diabetes
- arthritis
- osteoporosis
- chronic obstructive pulmonary disease (COPD)
- chronic kidney disease
- oral disease
54 per cent of all potentially preventable hospitalisations in WA are from select chronic conditions such as diabetes, asthma, angina, hypertension, congestive heart failure.
Supporting self-management can assist consumers to optimise their use of healthcare resources such as avoiding unncessary visits to hospital.
Determinants for chronic conditions
Determinants are factors that can influence how likely people are to stay well, or become ill or injured. Determinants can have a positive or negative impact on chronic conditions.
Those that have a positive effect are often referred to as protective factors. Those that have a negative effect are commonly referred to as risk factors.
Some determinants are modifiable, such as behavioural risk factors such as smoking, excess alcohol, inactivity, poor diet. Biomedical factors that are modifiable are excess weight, high blood pressure and blood cholesterol.
Non-modifiable factors include:
- age
- gender
- indigenous
- ethnic background
- family history
- genetic makeup.
Other broad influences for chronic conditions include:
- socio-economic
- psychosocial
- early life
- political factors.
Many chronic conditions are preventable, as well as respond more favorably to management and medical treatment in people who adopt healthy behaviours, such as:
- controlling body weight
- eating nutritious foods
- avoiding tobacco use
- limiting alcohol intake
- increasing physical activity.
Self-management strategies can be used to target modifiable risk factors and build the capacity and confidence of consumers to adopt healthier lifestyles. These strategies include behaviour change approaches, shared decision-making, goal setting and person-centred care.
Link between risk factors and chronic conditions
A table outlining the relationship between determinants and select chronic diseases has been compiled by the Australian Institute of Health and Welfare (external site).
It illustrates that chronic conditions that pose the greatest burden to society, share many common risk factors. Whilst some factors cannot be changed some are modifiable through behavioural and lifestyle change. Notably some risk factors overlap for conditions for example cardiovascular disease, Type 2 diabetes and chronic kidney disease. In some cases, one risk factor may be a precursor to another.
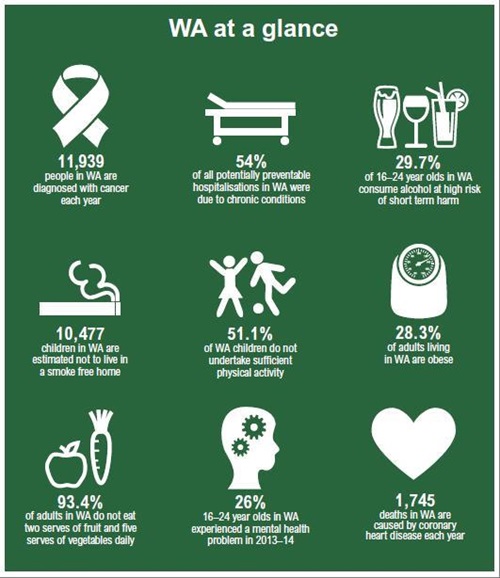
In WA, the occurrence of some risk factors, that are linked to chronic conditions, remains high as illustrated below.
WA Health Annual Report 2013–14
Aboriginal health
The high prevalence of chronic conditions experienced by Aboriginal people is significantly impacted by these determinants. Key factors influencing Aboriginal populations also include:
- historical impacts relating to loss of land and culture, and forced separation from family
- economic impacts such as unemployment, socio-economic status, access to housing, education and health and other services
- psychosocial/cultural impacts such as stress, disempowerment.
These risk factors although well documented, are complex and often result in Aboriginal people presenting to health services late in the course of their condition which can lead to significantly higher rates of complications.
Culturally and Linguistically Diverse (CALD) population groups
CALD communities include people that do not identify English as their primary language, or who are born into a culture significantly different to the Australian culture.
Migrants make up over one quarter of the WA population.
Refugee populations are at higher risk of lifestyle related health conditions as a result of exposure to displacement, poverty, food insecurity, torture and trauma.
What is considered to be a healthy lifestyle may be different from culture to culture. Culture, belief and context can also affect the way people respond to and manage their chronic conditions. Health information and skills therefore need to be communicated in a culturally appropriate manner, using an interpreter (family member or translator service) as required.
Migrants from some ethnic groups have higher prevalence rates of hospitalisations for several chronic and lifestyle related conditions, making them an important focus for health promotion and chronic condition self-management activities.
A number of CALD-specific support groups in WA provide assistance to adopt healthy lifestyles with:
- CALD-specific programs and services
- information and translated resources
- links to others in their communities.
Resources
Information sheets
Other resources
Produced by
Chronic Condition Self-Management